A 45-year-old man presents to the clinic for his annual exam. He has no remarkable medical history and does not take any medications on a regular basis. He has a strong family history of schizophrenia. He does not drink alcohol or use drugs but does report smoking approximately one pack per day for 3 years during his adolescence. He works as a school principal, is monogamous with his spouse, and notes no stressors. He reports no fatigue or issues with snoring. Vital signs include a BP of 120/76 mm Hg, HR of 72 bpm, RR of 16/min, T of 98.9°F, and BMI of 24 kg/m2, and he has a neck circumference of 15 in and abdominal circumference of 41 in. Laboratory evaluation includes a fasting blood glucose of 82 mg/dL, LDL of 96 mg/dL, HDL of 44 mg/dL, and serum triglycerides of 98 mg/dL. At this point, which of the following is this patient at most risk for developing in the future?
A Dyslipidemia B Insulin resistance C Schizophrenia D Sleep apnea E Total cardiovascular disease mortalityWaist circumference > 40 inches in men and 35 inches in women with or without a BMI ≥ 30 kg/m2 is defined as abdominal or central obesity and is an independent marker of visceral adiposity. Abdominal obesity is used as a criterion for the diagnosis of metabolic syndrome, which is linked to increased cardiovascular disease (CVD) risk, insulin resistance, and dyslipidemia. However, studies have shown that abdominal obesity alone can lead to a nearly twofold increased risk for total CVD mortality, prolonged QT intervals, and sudden cardiac death.
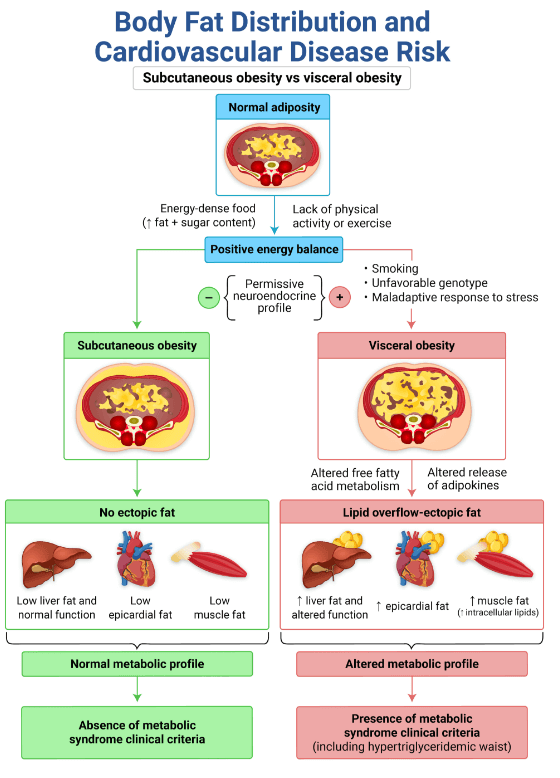
Given this patient’s normal blood pressure and laboratory evaluation, including his normal fasting blood glucose and serum triglyceride levels, he does not meet the diagnostic criteria for metabolic syndrome. Therefore, his risk is slightly less for developing dyslipidemia (A) and insulin resistance (B) as compared to his CVD risk.
A strong family history of schizophrenia or other behavioral health issues does increase an individual’s risk for behavioral health conditions. But schizophrenia (C) commonly occurs in adolescence and rarely presents in later life (over age 45 years).
The enhanced STOP-Bang (snoring, tiredness, observed apnea, high BP, BMI, age, neck circumference, male sex [formerly “gender,” but redefined to correctly reference biological sex]) (questionnaire can be used to determine an increased risk for sleep apnea (D)
. This patient is considered to have a low risk based on his only positive indicator of male sex.
Written and designed to help you understand the core concepts. Questions are just like you'll see on the actual exam, while explanations and illustrations focus on the essential information.
Give you a well-rounded perspective of your progress by illuminating any weaknesses, solidifying your strengths, and predicting your likelihood of passing the exam, so you can focus on the topics that need work.
“The most beautiful teaching images on the planet” help you further reinforce the core concepts. Visuals allow you to focus on meaning, group similar ideas, and make better use of your memory (and they're great to look at, too).
Personalized instruction from Content Education Experts who have been where you are and will help teach, uplift, and inspire you. It's like having a personal tutor!
Messages are answered by actual people—not bots—whose goal is to help and support you (with cheetah-like speed). Anything you need, we're here.
Want to revisit a helpful image or explanation? The search feature can help you quickly locate it. But you won't find any spoilers here—it searches content you've already seen.
Jennie is a family physician certified by the American Board of Obesity Medicine (ABOM) with a passion for overall health. She balances her professional life caring for hospitalized patients, reducing the chronic disease burden of obesity, and educating the next generation of physicians. With the new Obesity Medicine Qbank, Rosh Review learners will be prepared for success on the ABOM certification exam and able to provide evidence-based care in the field of obesity medicine.