Podcast Ep 19: Anaphylaxis, Diabetic Ketoacidosis, & More

Knowing is not enough; we must apply. Willing is not enough; we must do. -Johann Wolfgang von Goethe
Welcome back to episode 19! We are certainly relieved to have this year’s in-training exam behind us, and we are sure you are too. We hope you recognized some of the content we reviewed in episodes 1-15 and were able to grab a few extra points. Now that we’ve all had a brief break, we are back with new material to help you prepare for next year’s exam and to help improve your clinical acumen. It is important to keep reviewing all year-round.

- The Nexus criteria are used to rule out the need for cervical spine imaging. Use the mnemonic NSAID to remember the criteria: neurologic deficit, spinal tenderness, altered mental status, intoxication, and distracting injury.
- A pneumothorax can be identified on lung ultrasound by the absence of lung sliding.
- A simple pneumothorax, which is one involving less than 10% of the hemithorax, can be treated with a non-rebreather. Larger pneumothoraces will often require a chest tube or a pigtail catheter.
- The most common EKG finding for a myocardial contusion is sinus tachycardia. The most common course is a spontaneous resolution of the symptoms. However, with severe injuries, the most serious complication is delayed rupture.
Now onto this week’s podcast
Question 1
A 55-year-old man who is taking several antihypertensive medications presents to the ED with nausea, vomiting, shortness of breath, and a rash after eating a home-cooked Thai meal at a friend’s house about 1 hour ago. The symptoms began within seconds of the first bite of his meal. Despite the patient being administered 2 doses of intramuscular epinephrine, diphenhydramine, dexamethasone, and crystalloid fluids, his blood pressure remains at 75/38 mm Hg. Which other medication should be considered in this patient?
A. Cimetidine
B. Glucagon
C. Norepinephrine
D. Octreotide
Question 2
A 45-year-old woman with type 1 diabetes mellitus presents with fatigue in the setting of medication non-compliance. Her laboratory tests reveal a Na+ 125, K+ 3.1, chloride 97, bicarbonate 10, glucose 761, and pH 7.21. The patient is started on intravenous fluids. What therapy is most important to start next?
A. Hypertonic saline
B. Potassium repletion
C. Regular insulin
D. Sodium bicarbonate
Question 3
A 56-year old woman with a known left bundle branch block presents after a syncopal episode. EKG shows a regular, wide complex tachycardia with a rate of 160 beats/minute. Which of the following EKG features suggests a diagnosis of ventricular tachycardia over a diagnosis of supraventricular tachycardia with aberrancy?
A. Absence of AV dissociation
B. Capture and fusion beats
C. Irregular rhythm
D. QRS duration < 110 milliseconds.
Question 4
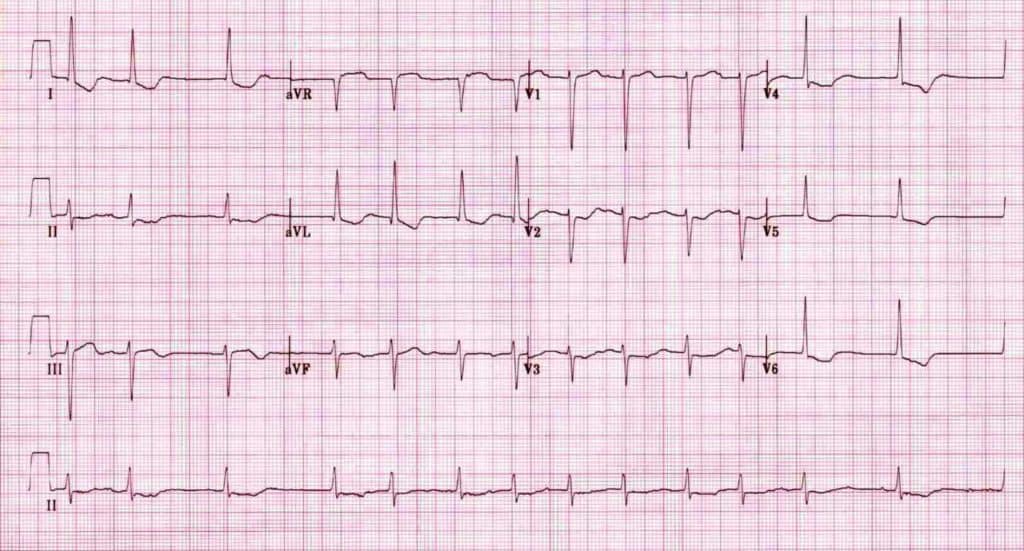
A 74-year-old woman with a history of congestive heart failure, hypertension, and coronary artery disease presents with confusion, abdominal pain, and nausea. Her medications include hydrochlorothiazide, aspirin, and digoxin. The patient’s ECG is shown above. She has a potassium level of 6.3 mEq/ml. Which of the following treatments should be initiated?
A. Activated charcoal
B. Calcium gluconate infusion
C. Digoxin immune Fab
D. Hemodialysis
Question 5
An 18-year-old woman with no significant past medical history falls while rock climbing and sustains a knee dislocation. Posterior tibial and dorsalis pedis pulses are unable to be palpated on the affected side. Her last meal was 2 hours ago. Which of the following statements is true regarding pre-procedural fasting?
A. Current fasting guidelines are based on results of randomized controlled trials comparing fasting status and incidence of aspiration
B. She is at risk of complications from knee dislocation and reduction should be performed regardless of fasting status
C. She should wait an additional 4 hours, until it is 6 hours since her last meal, since she is at increased risk of aspiration
D. Vomiting and loss of airway reflexes during procedural sedation is common
Question 6
A 32-year-old woman who is 8 weeks pregnant by dates presents to the ED with a 2-cm laceration to her index finger sustained while she was cutting a tomato. On review of systems, she also notes 2 days of vaginal spotting and lower abdominal cramping. Vital signs are within normal limits. Physical exam is consistent with a simple 2-cm laceration. The pelvic exam reveals a closed os and no adnexal tenderness or masses. Which of the following statements best describes the next step in management?
A. Delay treating her laceration until her pregnancy status is further clarified
B. Treat her laceration as indicated, and perform a beta-hCG quantitative level
C. Treat her laceration as indicated, perform a beta-hCG quantitative level, and obtain a pelvic ultrasound
D. Treat her laceration as indicated, then discharge with outpatient obstetrical follow-up

- Glucagon may be used for beta-blocker reversal.
- Common side effects of glucagon are vomiting, dizziness, hypokalemia, hyperglycemia, hypertension, and tachycardia.
- When treating DKA, replete potassium before starting insulin. Most protocols advocate for a potassium of at least 3.5 before starting insulin.
- Capture beats and fusion beats are indicative of ventricular tachycardia.
- A capture beat is a narrow complex supraventricular beat that is conducted within a run of ventricular tachycardia.
- A fusion beat is a beat formed from a supraventricular and ventricular impulse, resulting in a hybrid QRS complex.
- Digoxin toxicity can cause confusion, abdominal pain, nausea and vomiting as well as almost any type of dysrhythmia. PVCs are the most common EKG abnormality.
- The Salvador Dali mustache or scooped ST segments seen in patients on digoxin is indicative only of digoxin use and not toxicity.
- In digoxin overdoses, the potassium levels are helpful in prognosticating survival. A potassium level of > 5.5 mEq portends a worse outcome. The treatment is digoxin-specific antibody.
- Charcoal binds digoxin and can be given in acute overdoses if the patient has a normal mental status. There is no role for hemodialysis.
- Procedural sedation should not be delayed because the patient is not fasting. There is no good literature to suggest worse outcomes in those not fasting.
- In any pregnant patient with lower abdominal pain or vaginal bleeding, who does not yet have a confirmed IUP by ultrasound, a beta-hCG and pelvic ultrasound are required to rule out an ectopic pregnancy.
- Up to 20% of all pregnant patients will develop vaginal bleeding within the first 20 weeks of gestation. Of these, 50% will miscarry and the other 50% will go on to have a term pregnancy.
Thanks to Megha for the question suggestion. Remember to write “Roshcast” in the submit feedback box as you work through the question bank to flag questions you would like us to cover in future episodes.
For those of you thinking it is too early to start studying, do not forget there are 1200 questions in the Rosh review bank so you are better off starting sooner rather than later to get through it. Many of you already have the yearly subscription, so take full advantage by reviewing the questions there now. Lastly, follow us on Twitter at @Roshcast for updates and high-yield EM pearls in 140 characters or less!
Until next time,
Jeff and Nachi
P.S. Take a look at our most recent elite test-taker profile by Jennifer Bach.
Get Free Access and Join Thousands of Happy Learners
You must be logged in to post a comment.





Comments (0)