Podcast Ep 31: Ventricular Fibrillation, Traumatic Brain Injury, & More

The only journey is the one within.
-Rainer Maria Rilke
Welcome back to Episode 31! We are continuing our collaborative effort with the EM Clerkship podcast, focusing this week on tachydysrhythmias in addition to a mixture of random topics. We start the episode off with another rapid review of a few of the recent blog posts by Yehuda Wolf.

- In a gravid female, the uterus will be palpable at the umbilicus at around 20 weeks. At 12 weeks, the fundal height will be around the pubic symphysis. Lastly, at 36 weeks the fundus will be at the xiphoid process.
- Patients with polycystic ovarian syndrome are often obese and complain of hirsutism, irregular menses, acne, and sleep disordered breathing. You might also notice acanthosis nigricans and fatty liver disease.
- Management for PCOS is typically done in an outpatient setting, but a common regimen could include OCPs, metformin, and lifestyle modification.
Now onto this week’s podcast
Question 1
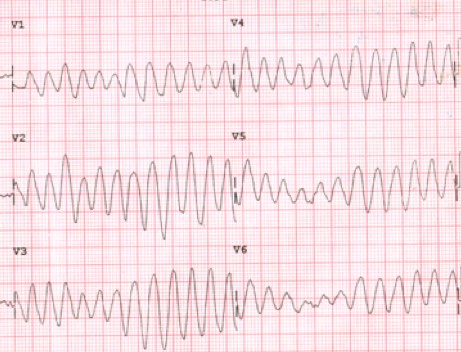
A 58-year old man is brought to the ED for chest pain that started 30 minutes prior to arrival while he was jogging in the park. Initially, the patient’s cardiac monitor shows sinus tachycardia with a rate of 120 beats per minute. However, while you are interviewing the patient in the resuscitation bay, he suddenly becomes pale, pulseless, and the below rhythm is seen on the cardiac monitor. Which of the following is the definitive next step to manage this rhythm?

A. Chest compressions
B. Defibrillation
C. Epinephrine
D. Synchronized cardioversion
Question 2
Which of the following treatments is contraindicated in a young person who has Wolff-Parkinson-White (WPW) syndrome with atrial fibrillation?
A. Adenosine
B. lbutilide
C. Procainamide
D. Synchronized cardioversion
Question 3
In a patient with traumatic brain injury, which of the following secondary insults should be given the highest priority for correcting in the ED?
A. Hypercarbia
B. Hyperpyrexia
C. Hypotension
D. Hypothermia
Question 4
A 45-year-old man with a history of opioid abuse presents to the ED with new onset syncope. While you are evaluating the patient, he becomes unresponsive and you note the rhythm below on the monitor. Which of the following medications is the most likely cause of this presentation?
A. Buprenorphine/naloxone
B. Fentanyl
C. Ketorolac
D. Methadone
Question 5
An 84-year-old man presents from a nursing home. The patient is lethargic and unable to provide any history. The transfer record reports a new cough and chills. His vital signs are T 102°F, BP 88/42, HR 118, RR 22, and oxygen saturation 95% on room air. In addition to an intravenous normal saline bolus of 30 cc/kg, which of the following is the most appropriate empiric treatment?
A. Cefepime, vancomycin, and azithromycin
B. Ceftriaxone and azithromycin
C. Ceftriaxone, vancomycin, and azithromycin
D. Ciprofloxacin and metronidazole
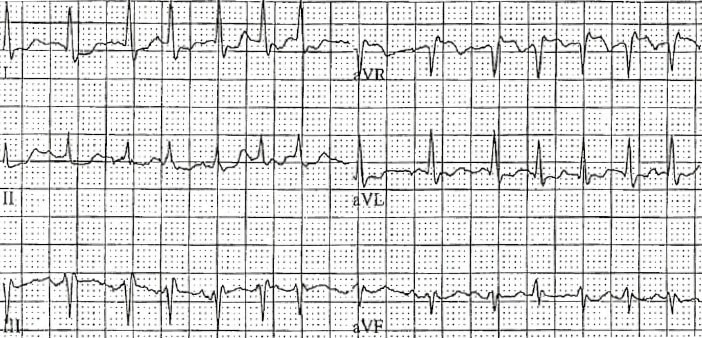
Question 6
What is the most likely underlying chronic medical problem in the patient with the following ECG?
A. Cardiomyopathy
B. COPD
C. Hyperthyroidism
D. Mitral stenosis

- In a witnessed cardiac arrest for a patient in ventricular fibrillation, immediate defibrillation should be performed.
- In an unwitnessed cardiac arrest with an unknown downtime, regardless of rhythm, chest compressions should be initiated immediately.
- The defibrillating dose for a biphasic defibrillator is 200 J, whereas 360 J are required with a monophasic defibrillator. Biphasic defibrillators are preferred as they cause less cardiac damage and have higher first shock success.
- In atrial fibrillation with WPW, avoid AV nodal blocking agents, like amiodarone, beta-blockers, calcium channel blockers, and digoxin.
- For an unstable patient in atrial fibrillation with WPW, synchronized cardioversion should be performed.
- In patients with traumatic brain injury, hypoxia and hypotension are associated with worse outcomes.
- Torsades de Pointes is often caused by drugs that prolong the QT. Other risk factors for Torsades de Pointes include female gender, hypokalemia, hypomagnesemia, structural heart disease, stroke, brain injury, and bradyarrhythmias.
- Torsades de Pointes should be treated with magnesium if the patient is stable. In an unstable patient, synchronized cardioversion or overdrive pacing should be performed.
- There are four criteria to think of for healthcare-associated pneumonia:
- Infection occurring within 90 days of a 2-day or longer hospitalization.
- Resident from a nursing home or long-term care facility.
- Infection within 30 days of receiving IV antibacterial therapy, chemo, or wound care.
- A patient on hemodialysis.
- HCAP should be treated with three drugs: one covering gram negatives including Pseudomonas, one for MRSA coverage, and lastly a third for atypical coverage.
- Always draw blood cultures before giving antibiotics when treating suspected sepsis and start a 30 cc/kg bolus assuming they do not have contraindications.
- Multifocal atrial tachycardia is often associated with COPD.
That wraps up Episode 31. Do not forget to follow us on Twitter @Roshcast and @Roshreview. We can also be reached by email at roshcast@roshreview.com. We are open to any feedback, corrections, or suggestions. You can also help us pick questions by identifying ones you would like us to review. To do so, write “Roshcast” in the submit feedback box as you go through the question bank. And finally, if you have a minute, make sure to rate us and leave comments on iTunes to help spread the word about Roshcast.
Until next time,
Jeff and Nachi
Get Free Access and Join Thousands of Happy Learners
You must be logged in to post a comment.





Comments (0)