Announcing the New Mock Internal Medicine Shelf/Clerkship Exam

Introducing the Mock Internal Medicine Shelf/Clerkship Exam, best suited for medical students who want to excel in their internal medicine clerkship.
The Mock Internal Medicine Shelf/Clerkship Exam is located in your Boost Box (on the home page of your desktop/laptop Rosh Review account). It contains 100 questions and comprehensive explanations to help you prepare for the NBME Internal Medicine Advanced Clinical Exam.
Categories covered include topics such as hypertension, diabetes, and hyperthyroidism with a few “zebras” to keep you on your toes.
Here is an example of a question and explanation:
A 45-year-old woman presents to the emergency room after a witnessed seizure at home. For the past week, she has had frequent headaches and severe pain on the left side of her head. Her past medical history is notable for depression and a dental infection treated about two weeks ago. She has no personal or family history of seizures. Blood cultures are negative. Which of the following is the most likely diagnosis?
A. Brain abscess
B. Intracranial infected aneurysm
C. Pyogenic meningitis
D. Septic cavernous sinus thrombosis
Answer A
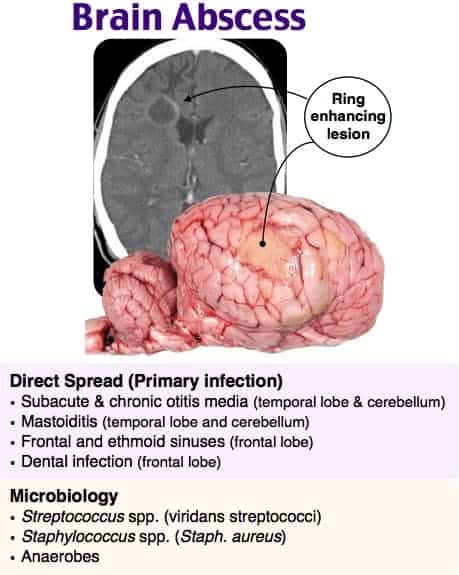
This patient has symptoms consistent with a brain abscess, or a focal infection inside the brain parenchyma. 20–60% of brain abscesses form through direct spread from a contiguous site and are typically single lesions. Common sites of origin include mastoiditis, dental infection, and otitis media. Hematogenous seeding is less common and usually results in multiple lesions. The most common organism identified in all brain abscesses is Streptococcus species. Patients with brain abscesses will often have nonspecific signs and symptoms. Only 20% of patients will have a triad of focal neurologic deficits, fever, and headache. Headache, usually on the side of the abscess and severe in quality, is the most frequently reported symptom. Less common findings include neck stiffness, vomiting, altered mental status, cranial nerve deficits, and papilledema. Seizures can be the first sign of a brain abscess and are seen in approximately 25% of patients. The diagnostic study of choice is magnetic resonance imaging. Once the presence of a brain abscess is confirmed, a specimen is gathered from surgery or computed tomography-guided aspiration. Treatment focuses on antibiotic therapy and surgical drainage. The estimated mortality in patients with brain abscesses is up to 30%.
An intracranial infected aneurysm (B) typically presents as a subarachnoid hemorrhage or stroke and is often seen in patients with endocarditis. Pyogenic meningitis (C) classically presents with the triad of fever, altered mental status, and nuchal rigidity. Blood cultures will be positive in the majority of patients with bacterial meningitis. Septic cavernous sinus thrombosis (D) is a rare infection of the cavernous sinus and can present with headache, cranial nerve deficits, periorbital edema, altered mental status, and diplopia. The absence of cranial nerve involvement and orbital findings makes a diagnosis of brain abscess more likely.
One Step Further question:
What is the most common neurologic sequela associated with brain abscesses?
Answer:
Seizures.
We also have mock shelf exams available for emergency medicine, family medicine, OB/GYN, pediatrics, and psychiatry. And be sure to check out our internal medicine board review question bank for thousands of comprehensive questions.
If you’re interested in How to Read ECGs Better Than a Cardiologist, How to Increase Your ABIM Internal Medicine Certification Exam Score by 100 Points, and other tips about all things internal medicine, head over to the Rosh Blog.
Study on,
The Rosh Review Team
Get Free Access and Join Thousands of Happy Learners
You must be logged in to post a comment.





Comments (0)