Rapid Review: Respiratory Distress Syndrome

Reviewed February 2024
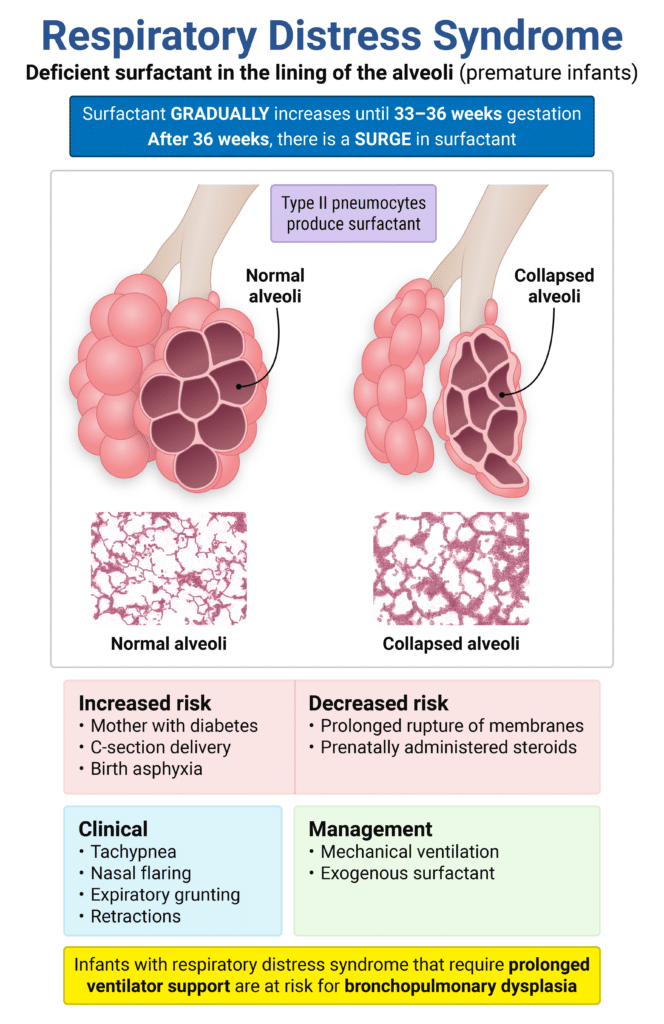
(Neonatal) Respiratory Distress Syndrome
- Patient will be a premature infant
- Respiratory difficulty within a few hours after birth
- PE will show tachypnea, tachycardia, cyanosis, nasal flaring, expiratory grunting, and chest wall retractions
- CXR will show decreased lung volume, air bronchograms, and a ground-glass appearance
- Diagnosis is made clinically and radiographically
- Most commonly caused by a deficiency of surfactant
- Treatment is O2, intubation, CPAP, surfactant
Sample question:
A newborn boy born at 32 weeks gestation is admitted to the NICU because of respiratory distress. He was born by cesarean section for breech presentation, premature labor, and rupture of membranes for approximately 2 hours. He weighed 1,845 g and appeared vigorous, with spontaneous respirations. His Apgar scores were 7 and 9 at 1 and 5 minutes, respectively. Shortly after birth, he developed respiratory distress. On examination, there are moderate subcostal retractions, shallow respirations, and bronchial breath sounds that are slightly diminished in intensity. The remainder of the examination is normal for the gestational age. The temperature is 37.2°C under radiant heat, heart rate is 119 bpm, respiratory rate is 75/min, blood pressure is 70/44 mm Hg, and oxygen saturation is 84–90% while the patient is breathing 50% oxygen with CPAP. Which chest X-ray finding is most consistent with the diagnosis?
Get Free Access and Join Thousands of Happy Learners
You must be logged in to post a comment.





Comments (0)